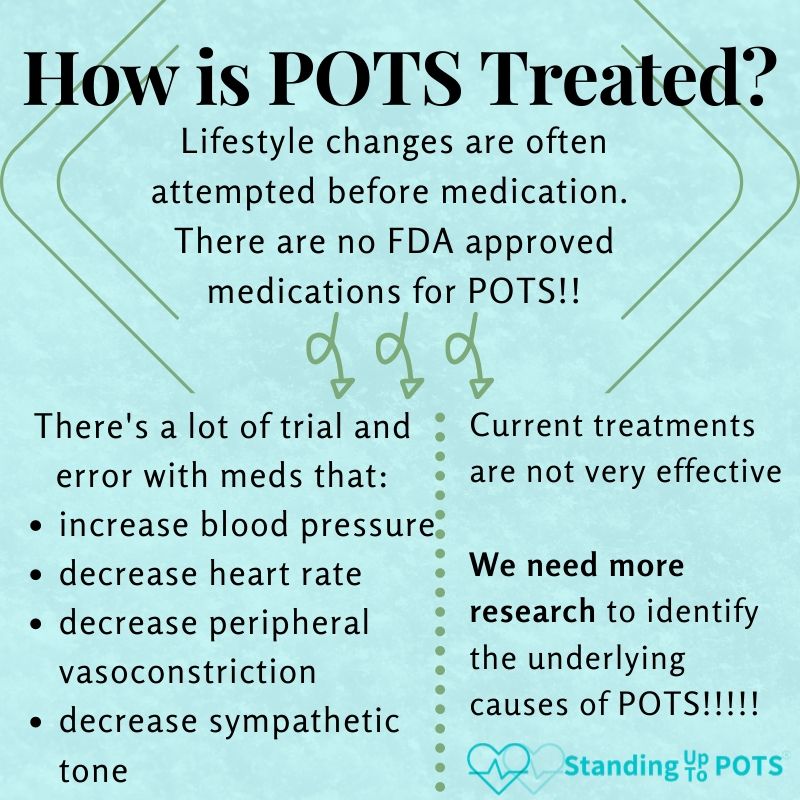
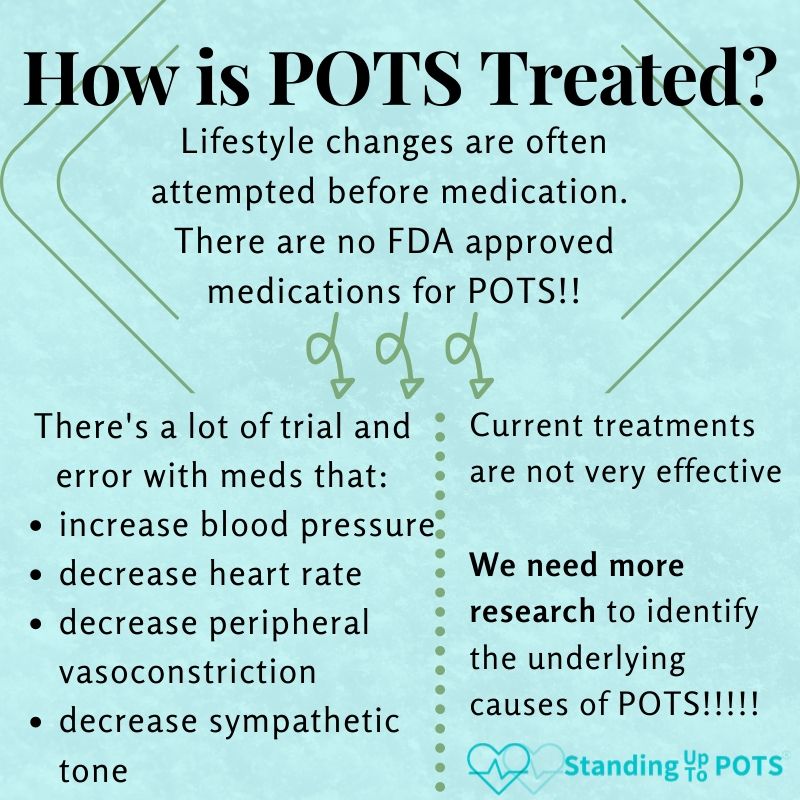
There is currently no cure for postural orthostatic tachycardia syndrome (POTS). These medications are prescribed off-label; meaning that they were designed for other disorders but have not been approved for POTS by the U.S. Food and Drug Administration. They may, however, help alleviate POTS symptoms and often require trial and error to find the best combination for individual patients. Here are some of the more common medications used to treat POTS symptoms.
Note: we are grateful to Dr. Artur Fedorowski, a top POTS physician-researcher and member of the SUTP Medical Advisory Board, for reviewing this page to ensure medications and dosages will be helpful for practitioners when treating their own POTS patients.
Heart rate controlling agents


Beta Blockers: Propranolol (Inderal; 10-40 mg TID; Fedorowski 2018); Bisoprolol (2.5 -10 mg once or twice daily)
Beta-blockers are especially recommended in hyperadrenergic subtype associated with sinus tachycardia > 120 bpm on standing (Fedorowski 2018). Beta blockers decrease heart rate, force of contraction, and conduction velocity through the heart. Beta blockers are most useful in people with elevated norepinephrine levels, beta receptor hypersensitivity, hyperadrenergic state and those suffering from angina, hypertension, or cardiac arrhythmias. A low dose of propranolol blunts the pounding fast heart rate feeling without lowering the blood pressure. However, beta blockers can reduce plasma renin activity and be counterproductive in those with low blood volume. Propranolol may be continued in pregnancy at 5 mg BID (Morgan et al. 2022).
Ivabradine: (2.5-7.5 BID; Raj et al. 2022)
Effective in people with low blood pressure or when beta-blockers are not well tolerated (Fedorowski 2018). This medication slows the heart rate and increases the amount of blood moved with each heartbeat. Not recommended for women who are pregnant or trying to get pregnant.
Verapamil: (40-80 mg BID/TID; Fedorowski 2018)
This calcium channel blockers can be effective for those with higher blood pressure, migraine, and chest pain (Fedorowski 2018). Some patients may suffer from so called “microvascular dysfunction” or coronary spasms in the heart producing angina-like symptoms, or, alternatively, from asthma, which may result in shortness of breath. As calcium channels blockers also relax small muscles in blood vessels and bronchi, dilating them, and simultaneously slow electrical activity in the heart to control heart rate, they might be tested in patients with POTS -associated unexplained chest pain and dyspnea. Adverse effects include blood pressure lowering, peripheral edema and slowing of peristaltic movements in the intestines.
Vasoactive and Volume-Expanding Agents
Centrally acting sympatholytic drugs: Clonidine (Catepres; 0.1-0.2 mg BID/TID; Raj et al. 2022)
Generally recommended for those with hyperadrenergic POTS and hypertensive tendency on standing (Fedorowski 2018). These medications decrease sympathetic activity and blood pressure. Clonidine works by stimulating the inhibitory alpha-2 adrenergic receptors in the medulla oblongata in the central nervous system. This reduces activity of the sympathetic nervous system and decreases heart rate, decreases release of renin, and dilates the blood vessels which reduces blood pressure. They can improve sleep when taken at bedtime.
Cholinesterase Inhibitors: Pyridostigmine Bromide (Mestinon; 10-60 mg BID/TID; Fedorowski 2018)
Particularly helpful in patients with suspected autonomic neuropathy, gastrointestinal dysfunction and non-specific muscle weakness (Fedorowski 2018). These are reversible inhibitors of the enzyme acetylcholinesterase that normally breaks down acetylcholine, the neurotransmitter of the parasympathetic nervous system. When acetylcholinesterase is inhibited, however, the level of acetylcholine increases in the synapse and is available to bind its receptor for a longer duration. Has been used safely in pregnancy for women with myasthenia gravis for decades and a dose of 30 mg BID may help women with POTS whose symptoms worsen during pregnancy (Morgan et al. 2022).
Mineralocorticoids: Fludrocortisone (Florinef; 0.1-0.2 mg daily; Raj et al. 2022)
Recommended for the hypovolemic subtype of POTS and those with low blood pressure. May worsen supine hypertension and hypokalemia (Fedorowski 2018). This is one of the most commonly prescribed medications for POTS. These steroids increase plasma volume and help the body retain both salt and water. They are often prescribed in tandem with salt tablets. This drug mimics aldosterone, which helps the body reabsorb sodium from the kidneys into the blood and secrete potassium into the urine. Florinef can deplete potassium and magnesium – supplements may be needed. Thermotabs can be helpful at supplementing both sodium and potassium when taking Florinef. It can also reduce levels of plasma renin activity and be counterproductive in those with low blood volume. The dose should never total more than 0.4 mg daily as adrenal suppression may occur. Fludrocortisone may be continued in pregnancy at 0.05-0.1 mg daily (Morgan et al. 2022).
Vasoconstrictors: Midodrine (ProAmatine; 2.5-10 mg TID; Fedorowski 2018); Droxidopa (100-600 mg TID may be also tested, but is contraindicated in pregnancy)
Effective in hypovolemic subtype of POTS and low blood pressure phenotype with pronounced orthostatic intolerance (Fedorowski 2018). This medication tightens the blood vessels to raise the blood pressure and decreases blood pooling in the legs and abdomen. It is short acting, however, and may need to be administered three times daily. It is best NOT to lie down to nap or sleep within four hours after taking this medication since the blood pressure can go up significantly when you are lying flat, but you can make an exception to this if you are feeling dizzy or faint. Midodrine can cause headaches and a feeling of goosebumps which is a good indication that the medication is taking effect. Midodrine may be continued in pregnancy at 2.5-5 mg three times daily (Morgan et al. 2022).
Antidiuretics: DDAVP (Desmopressin acetate; 0.1-0.4 BID; Fedorowski 2018)
This medication is a synthetic version of antidiuretic hormone, and helps the body retain water which can increase blood pressure. At night when you lay flat, the kidneys eliminate excess fluid. This is why many people with POTS often feel worse in the morning. By retaining some of the fluid at night, the blood pressure is higher in the morning which translates to feeling a bit better. This medication should be taken at bedtime.
1-2 L physiological saline infusion
In acute decompensated POTS, IV fluids can alleviate short-term symptoms (Fedorowski 2018). For more information, visit our page on IV fluids.
Treating Brain Fog and Fatigue
Stimulants: Dextroamphetamine (Adderall XR; 10-30 mg), Methylphenidate (Concerta 18-74 mg), Lisdexamfetamine (Vyvanse; 10-70 mg)
These are the same medications that can be used for individuals who have Attention Deficit Disorder. For POTS, they are used for those experiencing significant fatigue and brain fog. Stimulants have the added benefit of raising the blood pressure by vasoconstriction. These medications should be taken in the morning. One should start with the lowest dose taken in the morning (for instance, Attentin 5 mg; Elvanse 20mg) and increase the dose at one week interval if improvement does not occur. They should be discontinued in case adverse effects appear (tremor, anxiety, rapid heartbeat).
Modafinil (Provigil; 200 mg once daily)
This medication is not a stimulant but is used to improve wakefulness in patients with excessive sleepiness. It stimulates the brain and may work by increasing the amount of dopamine (a neurotransmitter used by neurons for communication) in the brain by reducing the reuptake of dopamine into neurons. This medication should be taken in the morning.
Other Common Medications
Low Dose Naltrexone (LDN; 0.001-16 mg, 4.5 mg is common)
This medication reduces pain and fights inflammation and has been used to treat a wide variety of disorders, including POTS. This competitive opioid receptor antagonist blocks the opioid receptor without activating it. LDN is generally taken before bedtime, unless it causes sleep disturbance, in which case it can be taken in the morning. Some experts believe LDN works best when exogenous opioids (e.g., processed foods, sugar, wheat, dairy) are minimized and vitamin D is replete. Because the dose is so small, it is necessary to get LDN from a compounding pharmacy.
Over-the-Counter Antihistamines if Suspect Mast Cell Activation Syndrome
In cases where the patient presents with signs of mast cell activation syndrome (MCAS) - facial flushing, hives, history of anaphylaxis, etc. - having the patient try a cocktail of antihistamines could be helpful. If warranted, patients could try cetirizine (Zyrtec; 10 mg) and famotidine (Pepcid AC; 20 mg) at breakfast and dinner, and diphenhydramine (Benedryl; 25 mg) at bedtime. If symptoms are reduced, further exploration into MCAS may be warranted.
Antidepressant medications
SSRIs: Paroxetine (Paxil) or Sertraline (Zoloft)
These medications can help people with POTS who are prone to fainting by raising the blood pressure and modifying the brain’s response to low blood pressure signals. They are also beneficial to those who have depression or anxiety issues.
Tricyclics: Amitriptyline (Elavil; 10-75 mg for neuropathic pain)
This antidepressant can be used as an adjuvant treatment for chronic neuropathic pain that is common in POTS and is helpful in 25% of cases (Moore et al. 2015).
Note: SNRIs can be detrimental to POTS patients. Avoid Bupropion (Wellbutrin), Desvenlafaxine (Pristiq), Duloxetine (Cymbalta), and Venlafaxine (Effexor) which fall into this SNRI category as they increase norepinephrine in the synapse and can increase sympathetic drive, already a problem for many POTS patients.